
To schedule a consultation, contact our NYC office at: 212.355.7017 today
| EARLIER DETECTION | WHAT IS DENSE BREAST? | GENE HEREDITY & TESTING | THE UNDERDIAGNOSED WOMEN |
| Women's Health Collaborative Podcast Host ALLIE FIEDERLEIN shares insight on her generation (GEN-Z) and the increasing numbers of breast cancer cases in our country. her age group also happens to be the next group that falls prey to being UNDERDIAGNOSED. Insurance companies and the medical community have made little or no action to support or identify the need for women in their 20's and 30's to be approved for standardized early detection / breast cancer screening. (L) WHC Podcast Episode 1: Watch an in-depth interview with "27 Year Old Stage 3 Breast Cancer Victim Survived - Despite of Docs Who MISDIAGNOSED!" (R) See Ms. Fiederlein's report on" "EARLIER DETECTION"- REACHING A GENERATION IN CRISIS" | |

WHY SCREEN EARLIER?
The women’s health community has identified 5-9% of all breast cancer cases occur in women between
the ages of 20 and 40.
- Women in younger ages may ignore signs like breast lumps or unusual discharges due to misconceptions about age propensity. This leads to delays in checkups and diagnoses.
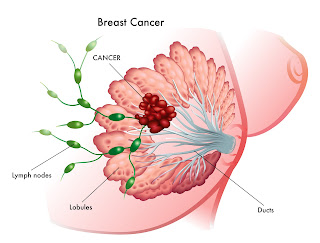
- Younger women are more likely to have dense breast tissue where standard mammograms are not recommended. Having dense breasts also carry an increased risk of breast cancer.
- Breast cancer treatments have been known to affect fertility, sexuality and pregnancy.
- Often coupled with unique issues, including concerns about body image, feelings of isolation, mental health support, and the financial burden of treatment and care.
Young women who are genetically predisposed may be at higher risk of breast cancer. Mutations in the BRCA1 or BRCA2 gene are common causes of hereditary breast cancers.
Bard Diagnostic Imaging offers a customized program for women under 40. Young patients will receive a comprehensive history assessment along with a BASE LINE scan using a case-specific mammography program. In addition, 3D Doppler Sonography is provided for additional & increased breast imaging accuracy as part of breast density detection. 3D Doppler imaging shows higher blood flow velocity, a common sign of cancerous activity in the breast. Studies have shown that suspicious blood flow identified by pre-surgery Power Doppler scans corresponds very well with the size, location and aggression of actual tumors that are then surgically removed. 3D sonography clearly shows tumor margins and 3D Doppler affords an index of cancer aggression and metastatic potential.

For over 30 years, Bard Diagnostic Imaging has been an active member of a national advocacy network for cancer prevention, education and research initiatives. This includes an alliance with the most recognized diagnostic imaging associations, women’s support resources and a professional community of top clinicians in the country. Women in younger age groups will benefit from access to these resources that offer a full understanding about the importance of early detection as part of a woman’s lifelong commitment to optimal wellness. For additional information, please visit our Women’s Health newsletter @ www.PinkSmartNews.com
"EARLIER DETECTION"- MY UNDERDIAGNOSED GENERATION IN CRISIS By: Alexandra Fiederlein (23) - Published in PINKSMARTNEWS.com 11/1/2023
 |
I belong to the graduate-level age group that continues to witness the increasing numbers of breast cancer cases in our country. The women in this generation also happens to be the next group that falls prey to being UNDERDIAGNOSED. Insurance companies and the medical community have made little or no action to support or identify the need for women in their 20's and 30's to be approved for standardized early detection / breast cancer screening. From the front-row perspective, younger women are as much at risk of getting cancer. Reports show an uptick in genetic predisposition for breast cancer*, alongside a dangerous attitude of denial. Addressing this calls for widespread education and screening programs in our community as essentials to a life of wellness and prevention.
Targeting the young working PROFESSIONAL is a major part of our population, where the vast majority tends to put off checkups and screenings because they are just "too busy". Professional women need to value their health above anything else, and therefore the narrative needs to be amplified in that area. We find this problem to be quite prevalent in urban areas with the constant on-the-go culture. Offering local resources and improved access for personal scanning are just some progress driven programs. GEN Z is a sensible focus group because these are the women who absolutely must receive routine scanning. We need to advocate for the narrative that age 40 is not the starting age where screening needs to begin- especially since we are now seeing cancer cases in younger ages are growing in numbers. Getting OB/GYN professionals on board is especially important because this is where women are getting their prescriptions.
If the drive for EARLIER DETECTION means proactive awareness, may this lead to turning social concern into clinical action. This includes clinicians joining hands with advocacy groups who recognize the many potential areas for at-risk women in my generation whose lives and safety continue to go unrecognized. And once the count of cancer cases and deaths rise exponentially due to inaction, perhaps then will the medical community find urgency in upgrading the required breast cancer screening age to (finally) include generations like mine.
Bard Diagnostic Imaging has been established in 1972- led by Dr. Robert L. Bard, internationally recognized as a leader in the field of 21st Century 3-D ULTRASONOGRAPHIC VOLUMETRIC DOPPLER IMAGING. Dr. Bard specializes in advanced 3-D sonography to detect cancers in numerous organs including the breast, prostate, skin, thyroid, melanoma and other areas. Dr. Bard’s images are used to accurately guide biopsies, target therapy and provide focused follow-up after treatment. Dr. Bard’s medical career began as a diagnostic radiologist and evolved into the practice of non-invasive 3D imaging with ultrasound, MRI and laser technologies. He has served in the military, been the head Radiologist at several leading hospitals, and published a multitude of textbooks and scientific papers. He presents articles worldwide, teaches at International Conferences and is on the Editorial Review Board of National and International Medical Journals. Holding medical licenses in several states, he holds Board certification from the American Board of Radiology (1974) and Fellowship in the American Society of Lasers in Medicine and Surgery (2014)
Bard Diagnostic Imaging is a supportive partner of the AMERICAN BREAST CANCER FOUNDATION, the NY CANCER RESOURCE ALLIANCE, THE WOMEN'S HEALTH COLLABORATIVE and the ARE YOU DENSE FOUNDATION. This New York-based facility is also an active partner of the INTEGRATIVE HEALTH RESEARCH CENTER / ANGIORESEARCH (501c3)
 |
 |
 |
 |
 |
 |
 |
In 2014, Imaging Technology News (ITN) introduced breast cancer survivor-turned-crusader Dr. Nancy Cappello and her story about having dense breast tissue leading to a late-stage cancer. A false negative mammography scan (diagnosed in 2004) concealed a large 2.5 cm suspicious lesion, which was later confirmed to be stage 3c breast cancer. This same cancer had metastasized to 13 lymph nodes. This sparked Dr. Cappello to create the "Are You Dense?" Foundation- an international awareness crusade to better support dense breast diagnostics and initiatives pass legislation to enact laws requiring mammography centers to inform patients about their breast density and the associated cancer risks. Dr. Cappello passed away on Nov 15, 2018, from secondary myelodysplastic syndrome (MDS), a bone marrow cancer that was a complication of her prior aggressive breast cancer treatments. But she ignited a legacy of fighting for improved policies, imaging technologies and advanced research to better address this health crisis that puts the est. 40% of the female population (women with dense breasts) at risk of a false negative reading.
 |
9/18/2023- As an Ob-Gyn physician and genomics specialist, I have spent the better part of 10 years translating research in the genomic and gene expression areas into clinically usable information for healthcare professionals. One of the biggest challenges we face when connecting research with patient care is the long delay in the translation process and dissemination of the information. It often takes 10 to 20 years for information (validated findings) that comes out of research to be applied in clinical practice. These delays result in many lost opportunities to provide better care for our patients. This is one of the reasons why I'm really passionate about accelerating this process and making it easier for clinicians and their patients to take advantage of cutting-edge information and new technologies.
 |
A QUANTITIATIVE ANALYSIS & IDENTIFYING THE KILLING CANCER
Written & produced by:
Dr. Robert Bard
I'm a radiologist subspecializing in ultrasound imaging, and I've been doing breast scanning for over 35 years. We have advanced radiology from x-rays to ultrasound to MRI and beyond. Reports are now promoting certain cancers should be considered as chronic diseases instead of "killing" cancers. We have known this for the past 30+ years that some cancers are dormant and while cancers are actively lethal. We've learned that some breast cancers are low-aggressive (but we need to continually watch them) or perhaps call for less aggressive treatment. We've also learned that certain cancers may surprise us; they do not follow the expected guidelines due to continung mutation. An example of this is the new findings of breast cancer cases in younger and younger ages (ie. 19 to 22 years old), and this age limit continues to get lower and lower. The same thing goes with breast cancers in men; five years ago, the count it used to be 1% of the population of cases, and now it's risen to 2% of the breast cancer population. We're finding more of it, partly thanks to better imaging access and partly because of improved awareness. Imaging innovations not only offers better detection but once we have the image, we can see if this is a "killing cancer" or not. The simplest technique and most basic technique is to use blood flow imaging. If we find many tumor vessels, "tumor's bad". If the tumor has only a few tumor vessels, tumor is "not so bad". More importantly, if you're treating a tumor and it goes from less to more, the treatment is not working. So we have a way of monitoring treatment in real time.